
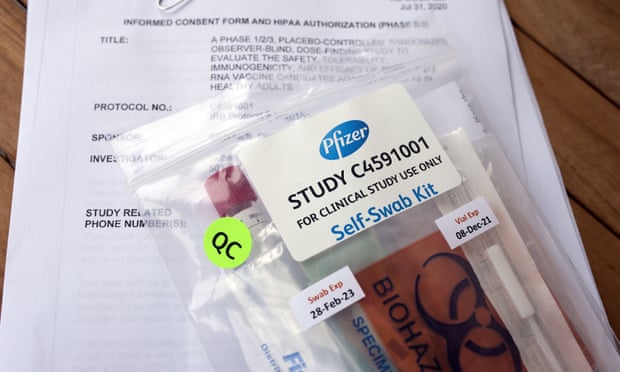
According to The Hill, pharmaceutical giants Johnson & Johnson and Eli Lilly announced on Oct. 12 and 13 that they are halting clinical trials for potential COVID-19 vaccines and treatments due to safety concerns and a possible vaccine-linked illness in a participant.
The Hill also says the halts are meant to allow time for an independent board of experts to sort through current data and determine if the illness reported is related to the treatments administered, in efforts to allow the board the opportunity to make an informed decision about restarting clinical trials. Experts said the public should be reassured by these decisions because it means the vaccine trial system is working as designed to protect patients.
Ashish Jha, dean of the Brown University School of Public Health, said during an interview with NBC’s Today Show on Oct. 14 that he was “heartened” by the news that the pharmaceutical companies were hitting speed bumps.
“I’m really heartened by these things. We’ve been racing so fast to develop therapies, vaccines, and we want to make sure the safety guardrails we usually have are in place. Seeing these pauses reminds me that the system is working, and when it gets through we’re going to be confident these things are safe,” Jha said.
Eli Lilly’s CEO David Ricks said on NBC Nightly News, “This should be very reassuring. These are the types of independent controls the industry builds into all of our work. Those have been built into COVID development, and we are committed to making sure that our COVID therapies are as safe and effective as any other therapy we’ve developed in the past.”
Elected officials and health experts that expressed concerns for public safety have been
The Johnson & Johnson announcement came one month after CNN obtained an internal safety report from pharmaceutical giant AstraZeneca, which detailed how a previously healthy 37-year-old woman who volunteered for the case study “experienced confirmed transverse myelitis” after receiving her second dose of the vaccine and was hospitalized on Sept. 5. According to the National Institution of Neurological Disorders and Stroke, transverse myelitis is an inflammation of the spinal cord, a major part of the central nervous system. The spinal cord carries nerve signals to and from the brain through nerves that extend from each side of the spinal cord and connect to nerves elsewhere in the body. The document, which is labeled as an “initial report,” describes how the study participant had trouble walking and experienced weakness, pain in her arms and other symptoms. Four days later, AstraZeneca dismissed media reports about the participant having a confirmed case of the rare neurological condition in which the spinal cord becomes inflamed.
Fox Business reports that this incident led to the launching of an investigation by the U.S. Food and Drug administration into the “unexplained illness,” causing the FDA to look into earlier trials of similar vaccines that were developed by the same scientists.
Sources familiar with the matter told Reuters that the government agency is looking to see if similar side effects emerged in these earlier trials, which were designed by researchers at Oxford University.
The Roll Call reports on Tuesday, Oct. 6, the White House is strongly encouraging a rush to develop a vaccine. This is causing immense pressure on the pharmaceutical companies to lower standards, with the intention of quickly pushing out vaccines. The FDA also had to issue long-awaited guidance on the data it received from pharmaceutical companies seeking emergency authorization of COVID-19 vaccines.
The 18-page guidance was released a day after reports suggested the White House had blocked the agency from issuing the guidelines, which are meant to increase public confidence in their ability to provide safe and effective vaccination. One of the issues addressed was whether the FDA would stick with its plan to require pharmaceutical companies to follow patients for two months after their final dose of a vaccine. The nonbinding FDA guidance and another document from the agency quietly released earlier maintained that standard. The pharmaceutical companies and regulators have been under intense political pressure to speed up the assessment and marketing of any potential inoculations, especially from President Donald Trump, who is seeking to deliver a vaccine to the American people as soon as next month.
For several weeks, FDA Commissioner Stephen Hahn has tried to reverse the politicization of the vaccine review process, saying any decision will be made by the agency’s career scientists without any outside influence.

Photographer: By Bill Clark/CQ Roll Call)
“We certainly want new products to come to the market as quickly as possible to help prevent additional illnesses and deaths, but if a national vaccine campaign is going to be successful, the American public must have full trust in the FDA’s review process,” he said Tuesday, Oct. 6, in a prerecorded speech at the Food and Drug Law Institute’s annual conference, The Roll Call reports.
While awaiting a vaccine, The New York Times reports that the White House is now embracing a declaration from scientists that oppose lockdowns and rely on “herd immunity.” According to Mayo Clinic, herd immunity occurs when a large portion of a community (or the “herd”) becomes immune to a disease, making the spread of disease from person to person unlikely. As a result, the community as a whole becomes protected when the portion of the group with the stronger immune system builds an immunity to the disease by creating antibodies that protect the more vulnerable of the population. Often, a certain percentage of the population must be capable of getting a disease in order for it to spread. This is called a threshold proportion. If the proportion of the population that is immune to the disease is greater than this threshold, the spread of the disease will decline. This is known as the herd immunity threshold.
There are two paths to herd immunity for COVID-19 — vaccines and infection.
Vaccines
A vaccine for the virus that causes COVID-19 would be an ideal approach to achieving herd immunity. Vaccines create immunity without causing illness or resulting in complications. Herd immunity makes it possible to protect the population from disease, including those who can’t be vaccinated, such as newborns or those who have compromised immune systems (i.e. the elderly or those with pre-existing, underlying conditions). Using the concept of herd immunity, vaccines have successfully controlled deadly contagious diseases such as smallpox, polio, diphtheria, rubella and many others.
The negative side of this approach is that herd immunity through vaccination sometimes has drawbacks, as protection from some vaccines can wane over time, requiring revaccination. Sometimes people don’t get all of the shots that they need to be completely protected from a disease.
Natural infection
Herd immunity can also be reached when a sufficient number of people in a population have recovered from a disease and have developed antibodies against future infection. For example, those who survived the 1918 flu (influenza) pandemic were later immune to infection with the H1N1 flu, a subtype of influenza A. During the 2009-10 flu seasons, H1N1 caused a respiratory infection in humans that was commonly referred to as swine flu.
However, there are some major problems with relying on community infection to create herd immunity to the virus that causes COVID-19.
First, it isn’t yet clear if infection with the COVID-19 virus makes a person immune to future infection. Research suggests that after infection with some coronaviruses, reinfection with the same virus, though usually mild and only happening in a fraction of people, is possible after a period of months or years. Further research is needed to determine the protective effect of antibodies against the virus in those who have been infected.
Second, even if infection with the COVID-19 virus creates long-lasting immunity, a large number of people would have to become infected to reach the herd immunity threshold. Experts estimate that in the U.S., 70 percent of the population, or an estimated 200 million people, would have to recover from COVID-19 to halt the epidemic. If many people become sick with COVID-19 at once, the health care system could quickly become overwhelmed. This could also lead to serious complications and millions of deaths, especially among older people and those who have chronic conditions.
In order for American citizens to slow the spread of the COVID-19 virus and protect individuals at increased risk of severe illness, health officials strongly recommend that we do the following:
- Avoid large events and mass gatherings: avoid close contact (with a 6 feet distance) with anyone who is sick or has symptoms of illness. That includes staying at home as much as possible and keeping distance between yourself and others, especially if you have a higher risk of serious illness. Keep in mind some people may have the COVID-19 virus and spread it to others, even if they don’t have symptoms or don’t know they have COVID-19.
- Wash your hands often with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer that contains at least 60 percent alcohol.
- Wear a cloth, non-medical mask to cover your face in public spaces, such as the grocery store, where it’s difficult to avoid close contact with others, especially if you’re in an area with ongoing community spread. Surgical masks and N95 respirators should be reserved for health care providers.
- Cover your mouth and nose with your elbow or a tissue when you cough or sneeze, and throw away the used tissue.
- Avoid touching your eyes, nose and mouth or sharing dishes, glasses, bedding and other household items if you’re sick.
- Clean and disinfect high-touch surfaces, such as doorknobs, light switches, electronics and counters daily.
- Stay home from work, school and public areas if you’re sick, unless you’re going to get medical care. Avoid public transportation, taxis and ride-sharing if you’re sick.


